—
HPI Network > HPI - Health Policy Institute > Lectures > Fee-for-services, per discharge payment for hospitalization and DRG (lecture 6/8)
Fee-for-services, per discharge payment for hospitalization and DRG (lecture 6/8)
Thursday, 27. June 2013, 12:06 — HPI
Watch the fourth lecture from 8 lectures course running under the title „Innovation for better healthcare” at University for modern Slovakia. In this lecture, Peter Pažitný and Angelika Szalayová talk about payment mechanisms in the health sector which defines behavior of health care professionals. In this episode, we talk about fee-for-services, per discharge payment for hospitalization and Diagnosis-related group (DRG). The lecture video includes English subtitles. Transcript together with the all schemas can be found under the video.
1. How are specialists, diagnostics and inpatient care facilities reimbursed?
Costs for specialists, inpatient care and diagnostic treatments make more than half of total healthcare expenditures:
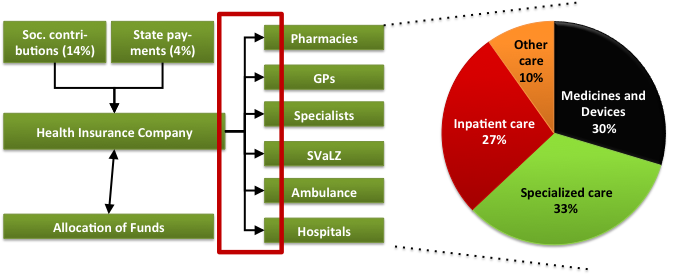
Source: prepared by the author
Three basic payment mechanisms are applied for acquiring specialized healthcare:
- Fee-for-service,
- Payments per diem (one day of hospitalization),
- Per discharge payments,
Each of these payment mechanisms have their deficiencies, therefore, all of them were continuously adjusted in order to avoid negative aspects.
2. What is a fee-for-service payment and how to determine a provider’s reimbursement?
With a fee-for-service mechanism, the provider charges health insurance companies for each patient visit and all treatments, which were provided during the examination and treatment. For instance, if a patient visits a cardiologist, who first examines him/her, conducts an ECG and then takes his/her blood, the doctor will at the end of the month charge the patient’s health insurance company for all treatments conducted: “Examining a single organ system”, “12 ECG leads” and “Taking blood”. There are thousands of such treatments in the list (while a specialized doctor uses mostly only a few tithes) and for each treatment there is value in the form of an exact number of points. Provider’s reimbursement is then calculated by summing up the points for each treatment provided to the insured of an insurance company during the period of one month, multiplied by the price for points, which has been negotiated for the specific period by the provider and the health insurance company. Using the point system for determining the value of treatments and prices for the points accumulated enables to change prices of treatments easily, while the difficulty of the treatments remains the same.
3. Where do we apply a fee-for-service mechanism in Slovakia?
Fee-for-services payments are applied for ambulatory specialists, laboratory and imaging diagnostics and also for some treatments in inpatient facilities – either for one-day surgeries (the patients leave the facility at the same day when arrived), or when the whole hospitalization lasts shorter than 3 days (keeping the patients two additional days at the facility after the surgery).
4. What does a fee-for-service system motivate for?
Due to the reason the provider is reimbursed for each treatment provided, this payment mechanism motivates him/her to provide the greatest number of treatments possible, also in cases patients do not need them (patients do not pay for these services directly, he/she does not care about undergoing for instance an additional magnetic resonance treatment). For the provider it might be even more beneficial to favor some treatments over other ones – if he/she provides them alone or if he/she has a higher income from specific treatments than from other.
5 How to improve fee-for-service payments?
The first reaction for avoiding such motivations of the fee-for-service payments was the introduction of the so-called limits. Each provider received a maximum budget for a month for treatments provided, and if these limits were exceeded, the provider could not receive more resources from the insurance company. This measure should have motivated him/her to provide only those services that were really needed. However, in practice it rather looked like doctors continued providing the same amount of services than before and when they ran out of the limit at the end of the month, they refused to accept more patients and some of them also closed their practices. These “higher limits” (i.e. for treatments provided after exceeding the limits, but not reimbursed) became subject of conflicts at the end of the year. The problem of limits is that they were set according to the past performance of the provider and not according to objective criteria (such as professionalism of the provider, number of patients and their sickness). Thus, limits were higher for those providers, who conducted unnecessary treatments before the introduction of limits.
Such limits exist also nowadays, especially in laboratory and imaging diagnostics, however, the fee-for-service system for ambulatory specialists has changed to a so-called regressive price for points. The provider has also a set budget for the period of one month, however, after exceeding these limits, the price of additional treatments does not decrease to zero, but to lower prices than the original ones. This approach is based on the fact that after exceeding a specific number of treatments, providers’ expenditures are lower for providing additional treatments (marginal costs), because he/she already covered the fixed cost. In case of some insurance companies the price of points after exceeding limits decreases only if the provider does not fulfill the agreed quality and effectiveness criteria.
6 What are per diem and per discharge payments for hospitalization and how do we set the reimbursement for the provider?
For inpatient care in Slovakia, besides fee-for-service payments, there are two additional payment mechanisms to be applied: per diem payments and discharge payments for hospitalization. For per diem payments the hospital receives a fixed amount for each day a patient stays in the facility. Applying a discharge payment for hospitalization a fixed amount is reimbursed disregarding the number of days spent by the patient in the hospital.
7. What do per diem payments and discharge payments for hospitalization motivate for?
Per diem payments motivate healthcare providers to keep patients in the facility as long as possible, even more than needed, because the last unnecessary days spent in the hospital are the most profitable for the provider (costs for treating an almost healthy patient are the lowest, while the reimbursement from the health insurance company is the same as at the beginning of the hospitalization). For discharge payments for hospitalization the provider is, on the contrary, motivated to release patients as soon as possible, even sooner than his/her health status would allow.
Both payment mechanisms motivate healthcare providers to accept patients with lighter diagnoses, for which they profit the most, while “more costly” patients can be sent to other facilities.
8. Where are per diem payments and discharge payments for hospitalization applied?
Per diem payments are currently used very rarely, especially during long term hospitalizations, when patients spend weeks or months in hospitals. Discharge payments for hospitalization are the most frequently used payments for inpatient care in Slovakia.
9. How can per diem and discharge payments for hospitalization be improved?
Also in case of payments for hospitalization, some health insurance companies use limits in order to restrict the maximum amount of financial resources provided to the healthcare provider. Another approach is to plan and manage hospitalization, when the provider announces each acute hospitalization to the health insurance company by 24 hours after accepting the patient. Hospitalizations, which can be postponed, are also announced to the health insurance company before accepting the patient for hospitalization. The health insurance company then approves only the amount of those planned hospitalizations, which correspond to virtual limits. A more significant improvement of payments for hospitalization would be the introduction of DRG.
10. What is DRG?
DRG (diagnosis related groups) is a classification system, which groups cases of short-term hospitalization (hospitalization episodes) to one of several hundred groups according to clinical and cost similarity.
In one DRG group all hospitalization episodes are grouped, which are also clinically and cost-wise homogenous enough.
11. What is the asset of DRG?
The asset of DRG is that it
- measures the production of hospitals
- reimburses hospitals in a more justified way – it removes horizontal and vertical injustice of payments
- introduces a superior way to compensate for the more risk structure of patients (DCG predictor)
12. DRG as a classification mechanism
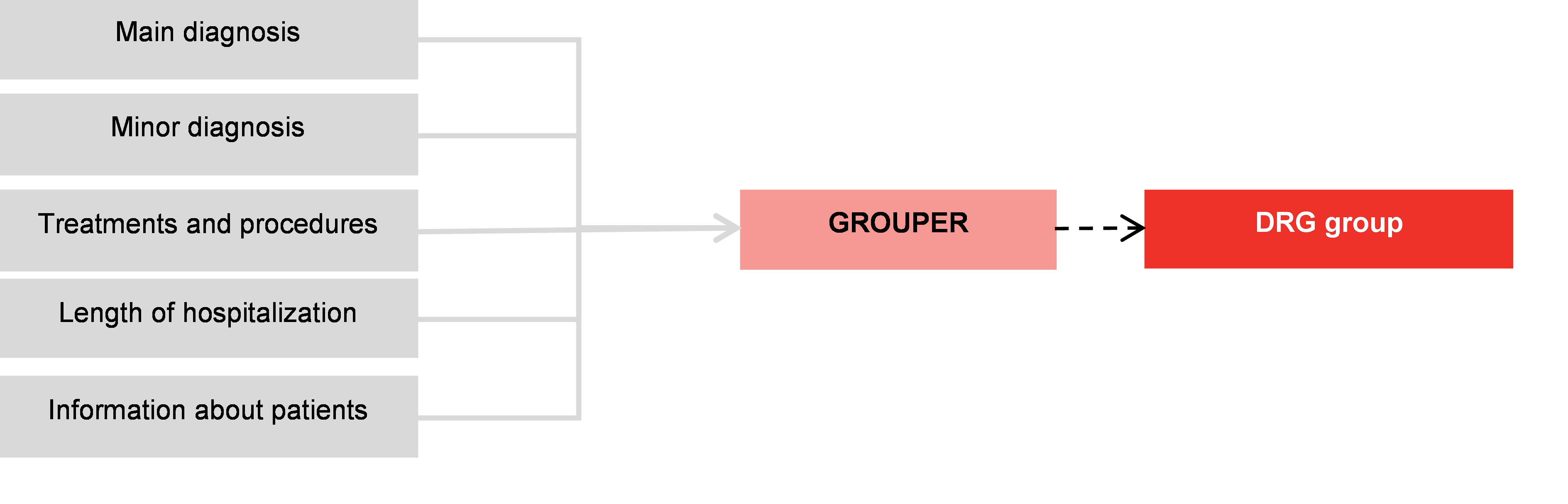
Source: prepared by the author
13. DRG as payment mechanism
The importance of DRG is that the prospective rate (risk-priced) can sufficiently deteriorate the producer from producing services for higher costs as would be accepted by the free market.
The prospective set rate is derived from the assumed average costs of the particular DRG group.
This means to a priori capping payments for units and creating production risks for providers, which cannot produce at higher costs than the regulated reimbursement.
14. What is the relative weight?
Each DRG group has its own relative weight, for instance a particular DRG within the MCD 05 group – cardiovascular diseases.
|
Particular DRG within the MCD 05 group – cardiovascular disease |
DRG weight |
|---|---|
|
Angina pectoris, arthrosclerosis and other cardiovascular diseases |
0.68230 |
|
Angina pectoris with complex un-invasive diagnostic procedures |
0.89730 |
|
Acute myocardial heart attach treated with special treatments |
1.81635 |
|
Acute myocardial heart attack with implementing a temporary pacemaker |
2.42426 |
|
Acute myocardial heart attack treated with thrombotic therapy |
2.72841 |
|
Acute myocardial heart attack treated with PTKA without stent |
5.90909 |
|
Acute myocardial heart attack treated with PATKA with stent |
8.88757 |
Source: Hungarian DRG
15. What is the basic rate?
Basic rate is the rate for DRG with a relative weight of 1, for instance 1.000 €.
16. What is the length of hospitalization?
Each DRG group has a set minimum and maximum length of hospitalization, for not complicated cases, for slightly complicated cases and for complicated cases. Minimum and maximum length of hospitalization influence the overall amount of reimbursement.
17. How to calculate the reimbursement in a DRG system?
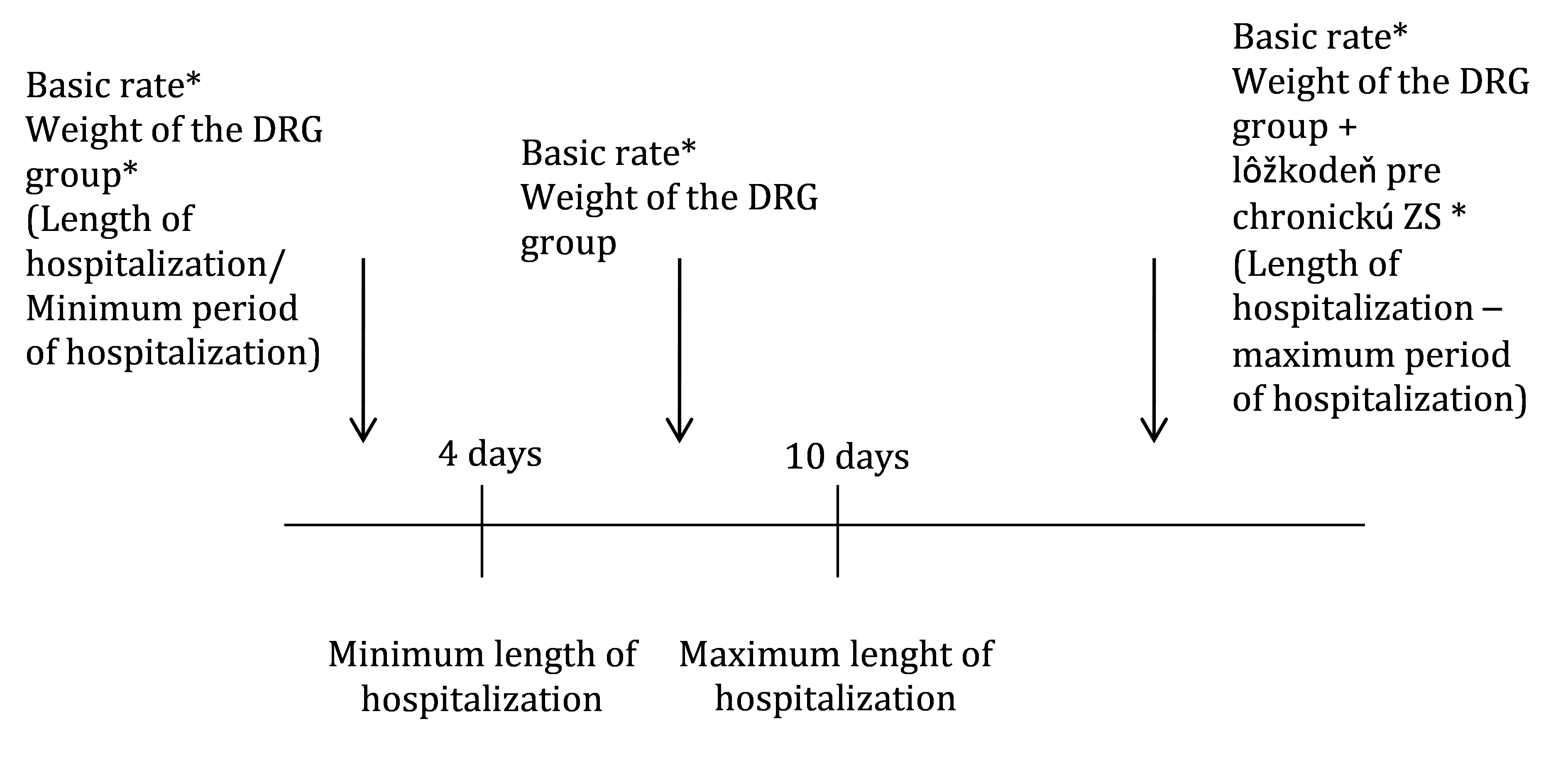
Source: prepared by the author
An example of reimbursement in a DRG system
|
Basic rate for a DRG group with the weight of 1 |
Weight of the DRG group |
Real length of hospitalization |
Reimbursement |
|---|---|---|---|
|
1.000 € |
1.50000 |
7 days |
1.500 € |
|
1.000 € |
1.50000 |
2 days |
750 € |
|
1.000 € |
1.50000 |
13 days |
1.500 € plus the daily fee for 3 days (if 30 € per day), the total amount is 1 590 € |
Source: prepared by the author
Summary
-
When acquiring specialized healthcare, health insurance companies in Slovakia apply 3 basic payment mechanism:
- Fee-for-service
- Payments per diem
- Discharge payments for hospitalization
- Applying a fee-for-service payment, healthcare providers charge the health insurance company for each patient visit and for each treatment from a list that was provided during the examination to the patient.
- Applying per diem payments, the hospital receives a fixed amount for each day spent by the patient in the hospital.
- Applying discharge payments for hospitalization a fixed amount is paid for the whole hospitalization of the patient, disregarding the number of days spent by the patient in the hospital.
- DRG (diagnosis related groups) is a classification system, which groups cases of short-term hospitalization (hospitalization episodes) to one of several hundred groups according to clinical and cost similarity. Key components of DRG are: Grouper, relative weights, basic rates, minimum and maximum days of hospitalization.
News
The amendment of the Decree on emergency medical service
Health insurance companies returned over 400 thousand €
The HCSA received 1,647 complaints last year
A half million people will earn more
Most of public limited companies ended in the black
Debt of hospitals on premiums has grown to nearly € 105 MM
Slovak health care may miss € 250 million next year
Profits of HIC amounted to € 69 mil. last year
Owners of Dôvera paid out money but did not paid taxes
Like us on Facebook!
Our analyses
- 10 Years of Health Care Reform
- New University Hospital in Bratislava
- Understanding informal patient payments in Kosovo’s healthcare system
- Analysis of waiting times 2013
- Health Policy Basic Frameworks 2014-2016
- Analysis of informal payments in the health sector in Slovakia
- Serbia: Brief health system review
developed by enscope, s.r.o.
